Infection Control: Setting a High Bar
Liz Weingast, Our Vice President for Clinical Excellence and Gerontological Nurse Practitioner, Speaks About Protecting Patients and Staff in the Age of COVID-19.
Keeping patients safe has always been a priority at The New Jewish Home. What changes did you have to make with the arrival of COVID-19?
We are being so cautious about hand hygiene, about personal protective equipment, about ensuring the cleanliness of the area. Not that these things weren’t happening before, but the routine has become much more robust. By regulation, each of our nursing homes must have an infection-prevention registered nurse on staff — a specialist responsible for looking out for new infections and for managing the risks. But in the era of COVID you can’t just have one person; infection control is now intertwined in all our jobs.
With several months of COVID behind you now, can you reflect on how your infection- control efforts are succeeding and why?
We are fortunate to have a cohesive leadership team headed by our President and CEO, Dr. Jeffrey Farber, who is also a geriatrician. Most organizations that care for older adults are not led by medical doctors. Dr. Farber ensures that providing exceptional clinical care is our first priority. Early on in the pandemic, we were being slammed with new information every ten minutes, but with topnotch clinicians to guide us, we were able to make educated decisions based on the latest information and research. We are privy to learning about the clinical protocols used at Mount Sinai and apply those that are appropriate at our facility. Perhaps most important, from Day One, we had one individual, Dr. Ruth Spinner, our Manhattan Medical Director, overseeing our system-wide COVID response. Having a point person — a doctor rather than an administrator — coordinating every aspect made a huge difference. Not all nursing homes have that capacity.
What were the very first steps you took after the pandemic began?
We immediately began working very closely with the New York State Department of Health (DOH) epidemiology team; they came on site and advised us. We put droplet and contact-isolation precautions in place very quickly.
What exactly does that mean?
With a respiratory illness, care providers use so-called droplet precautions to protect themselves and others. Typically, you make sure the person who is ill is isolated and that you are using a mask when you’re in their room. With COVID-19, the Centers for Disease Control and Prevention (CDC) early on recommended enhanced droplet precautions which means wearing not just masks, but also eye protection — those face shields you see on TV — as well as protective gowns and gloves, which are disposed and proper hand hygiene is practiced before you go to the next patient. That’s the personal protective equipment (PPE) that has been so much in the news.
What we usually hear about is shortages of PPE. Did you have that issue?
The usual paths of obtaining PPE really dried up quickly, but we made rigorous efforts to find creative ways to secure the equipment we needed. We were fortunate that our hard work paid off. Our staff always had the PPE needed to safely provide care.
In addition to using PPE, you mentioned isolating patients. How does that work?
The idea is to keep the illness contained. Early on, we created a unit for people with COVID-19 and when someone got sick, we moved them out of their regular room onto that unit. When they recovered and tested negative twice, we moved them back to their home unit.
What about group activities such as classes, workshops, religious services and social gatherings?
We’re thankful that now we’re able to offer small group therapeutic recreation programming and religious services, while adhering to social distancing guidelines. Residents are once again enjoying our beautiful gardens. At the height of the pandemic, the rabbis at our Manhattan and Westchester facilities broadcasted daily uplifting messages and music, and it made a real difference for our residents, as well as our staff.
How do you prevent infection from coming in from outside?
The only people who may enter our facilities at the moment are those directly involved with running the building or caring for the people who live there. The DOH recently began allowing limited visitation, and as most nursing homes in the state, we are working towards meeting the conditions to welcome families and loved ones back. Since March, all staff have to fill out a questionnaire about their health status and get their temperature taken at each shift. In May we began giving all employees weekly swab tests. In addition, we brought on extra housekeeping staff to clean high-touch surfaces more frequently.
Are you able to admit new patients?
We do accept new patients. They need to test negative for COVID-19 before they are admitted. Once they arrive at The New Jewish Home, they’re tested for the disease again and they’ll go to a unit where they will be isolated for 14 days in a private room. During the two-week period, new patients will receive rehabilitation in their rooms. We require, as part of our own protocol, a second negative test before they are taken off isolation. I want to note that this is an extra precautionary step that Jewish Home has decided to administer for the safety of our new and existing clients; there are other nursing homes that do not test after 14 days.
What would you say to a patient who may feel apprehensive about going to a rehab facility at this time?
I can’t think of a better place to get well and go home. In some ways we’re even safer than hospitals. Our staff members are tested weekly for COVID-19 and we have strict infection control protocols in place. As I mentioned earlier, patients are in private rooms, we test patients once they arrive and again after 14 days. And our rehabilitation programs are excellent—our clinicians are extremely skilled and passionate about their work. You may have heard about “Miracle Larry” recently in the news. We’re proud to have helped him return home after regaining his health and strength in our rehab program.
Nearly six months down the road, how would you assess your efforts at infection control?
Right now, in July, we’re celebrating zero cases at both our Manhattan and Westchester facilities. I attribute this achievement to our stringent infection control efforts. So we’re headed in the right direction. But we are not letting down our guard because this virus has proven to be so unpredictable, and we know it’s not over.
You have been at The New Jewish Home for more than two decades. What has it meant to you personally and professionally to help guide the institution, the patients the staff through the pandemic?
Older adults have complex sets of care needs — more so during the era of COVID-19. When I studied to become a nurse practitioner in geriatrics, I saw how older adults and their needs were so little valued in the hospital, which is what brought me here. I find great value in learning from the people I’ve cared for. Their life experience and how they cope with challenges never ceases to enrich my life. From a professional perspective, The New Jewish Home has given me wonderful opportunities to merge my clinical expertise with becoming a leader on the corporate level. Extraordinary colleagues have contributed to my knowledge and enjoyment of my work. What they have in common is a commitment to the mission of the organization and a love for those we serve. That’s what makes Jewish Home such a special a place to work.
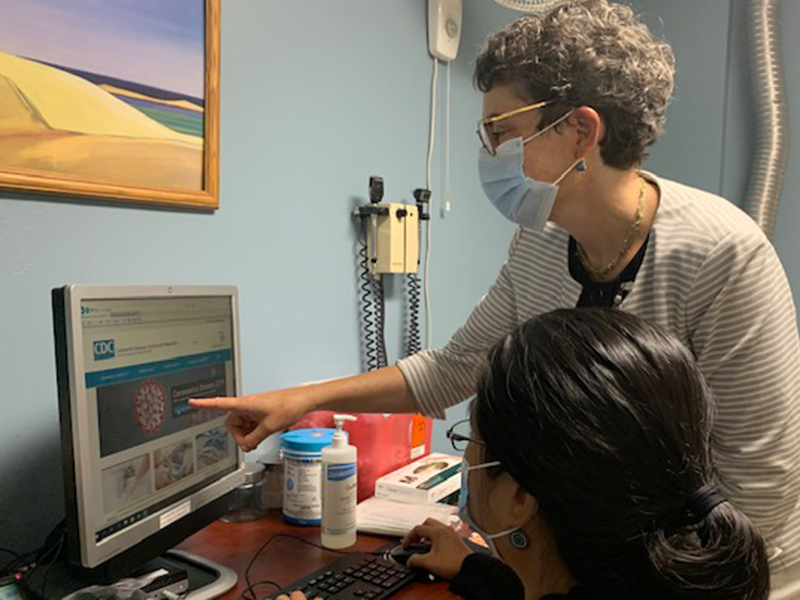
Photo caption: Liz Weingast, VP for Clinical Excellence and Sheila Molarto, Quality Assurance & Performance Improvement Nurse Manager working on Occupational Health and Safety during the time of COVID-19.
The New Jewish Home has a proud legacy of empowering older adults to live with purpose and enhanced well-being. We’ve been around since 1848 as one of the nation’s first nursing homes, and now serving older New Yorkers of all backgrounds through a portfolio of health care services, including post-acute care and rehabilitation, skilled nursing, adult day care, assisted living, and at-home care.
See how we continue to elevate health care for older adults through our Research Institute on Aging and our SkillSpring program (formerly known as Geriatrics Career Development program), which empower teens and young adults to begin careers in health care.